Hypothyroidism

Hypothyroidism
Background Hypothyroidism is a common endocrine disorder resulting from deficiency of thyroid hormone. It usually is a primary process in which the thyroid gland is unable to produce sufficient amounts of thyroid hormone. Hypothyroidism can also be secondary—that is, the thyroid gland itself is normal, but it receives insufficient stimulation because of low secretion of thyrotropin (ie, thyroid-stimulating hormone [TSH]) from the pituitary gland. This generally occurs in the presence of other pituitary hormone deficiencies. In tertiary hypothyroidism, inadequate secretion of thyrotropin-releasing hormone (TRH) from the hypothalamus leads to insufficient release of TSH, which in turn causes inadequate thyroid stimulation. But this rarely happens. Worldwide, iodine deficiency remains the leading cause of hypothyroidism.
In the United States and other areas where iodine intake is adequate, the most common cause is autoimmune thyroid disease (Hashimoto’s disease). Hypothyroidism can also be caused by drugs or other iatrogenic factors. (see Etiology) Some, but not all, studies suggest that low vitamin D levels may be linked to autoimmune thyroid diseases such as Hashimoto’s thyroiditis and Graves’ disease. However, intervention studies to date have not demonstrated the benefits of supplementation. No association was found between vitamin D levels and thyroid cancer. This is still an area of investigation.
The patient’s condition ranges from asymptomatic to myxedema coma with multisystem organ failure. Because thyroid hormones are required for almost all metabolically active cells, a deficiency in these hormones can have a variety of consequences. (See presentation.) Third-generation TSH assays are readily available and are generally the most sensitive screening tools for primary hypothyroidism. The generally accepted reference range for
normal serum TSH levels is 0.40 to 4.2 mIU/L. If your TSH levels are above the reference range, the next step is to measure free thyroxine (T4). Subclinical hypothyroidism, also called mild hypothyroidism, is defined by normal serum free T4 and triiodothyronine (T3) levels and mildly elevated serum TSH concentrations. Like clinical hypothyroidism, Hashimoto’s thyroiditis is the most common cause of subclinical hypothyroidism in the United States.
In hypothyroidism, thyroid hormones are prescribed to supplement or replace endogenous production. In general, hypothyroidism can be adequately treated with regular daily administration of levothyroxine (LT4). (See Treatment and Medicines) Congenital hypothyroidism, which affects 1 in 4,000 newborns, is caused by a congenital malformation of the thyroid gland (see Pediatric Hypothyroidism). This disorder is included in newborn screening programs in the United States and many other countries and is easily treatable once detected. Cretinism refers to severe hypothyroidism in infants and young children. This is usually caused by maternal iodine deficiency, but fortunately this is becoming less common.
Hypothyroidism (also called underactive thyroid, low thyroid or hypothyreosis) is a disorder of the endocrine system in which the thyroid gland does not produce enough thyroid hormone. It can cause a number of symptoms, such as poor ability to tolerate cold, a feeling of tiredness, constipation, slow heart rate, depression, and weight gain. Occasionally there may be swelling of the front part of the neck due to goitre. Untreated cases of hypothyroidism during pregnancy can lead to delays in growth and intellectual development in the baby or congenital iodine deficiency syndrome.
Worldwide, too little iodine in the diet is the most common cause of hypothyroidism. Hashimoto’s thyroiditis is the most common cause of hypothyroidism in countries with sufficient dietary iodine. Less common causes include previous treatment with radioactive iodine, injury to the hypothalamus or the anterior pituitary gland, certain medications, a lack of a functioning thyroid at birth, or previous thyroid surgery. The diagnosis of hypothyroidism, when suspected, can be confirmed with blood tests measuring thyroid-stimulating hormone (TSH) and thyroxine levels.
Salt iodization has prevented hypothyroidism in many populations. Thyroid hormone replacement with levothyroxine treats hypothyroidism. Medical professionals adjust the dose according to symptoms and normalization of the thyroxine and TSH levels. Thyroid medication is safe in pregnancy. Although an adequate amount of dietary iodine is important, too much may worsen specific forms of hypothyroidism.
Worldwide about one billion people are estimated to be iodine-deficient; however, it is unknown how often this results in hypothyroidism.In the United States, hypothyroidism occurs in 0.3–0.4% of people. Subclinical hypothyroidism, a milder form of hypothyroidism characterized by normal thyroxine levels and an elevated TSH level, is thought to occur in 4.3–8.5% of people in the United States. Hypothyroidism is more common in women than in men. People over the age of 60 are more commonly affected. Dogs are also known to develop hypothyroidism, as are cats and horses, albeit more rarely. The word hypothyroidism is from Greek hypo- ‘reduced’, thyreos ‘shield’, and eidos ‘form’.
Signs and symptoms
People with hypothyroidism often have no or only mild symptoms. Numerous symptoms and signs are associated with hypothyroidism and can be related to the underlying cause, or a direct effect of having not enough thyroid hormones. Hashimoto’s thyroiditis may present with the mass effect of a goitre (enlarged thyroid gland). In middle-aged women, the symptoms may be mistaken for those of menopause.
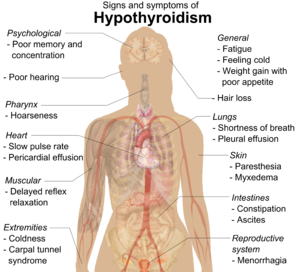
| Symptoms | Signs |
|---|---|
| Fatigue | Dry, coarse skin |
| Feeling cold | Cool extremities |
| Poor memory and concentration | Myxedema (mucopolysaccharide deposits in the skin) |
| Constipation, dyspepsia | Hair loss |
| Weight gain with poor appetite | Slow pulse rate |
| Shortness of breath | Swelling of the limbs |
| Hoarse voice | Delayed relaxation of tendon reflexes |
| In females, heavy menstrual periods (and later light periods) | Carpal tunnel syndrome |
| Abnormal sensation | Pleural effusion, ascites, pericardial effusion |
| Poor hearing | |
| Muscle weakness |
Delayed relaxation after testing the ankle jerk reflex is a characteristic sign of hypothyroidism and is associated with the severity of the hormone deficit.
Myxedema coma
Myxedema coma is a rare but life-threatening state of extreme hypothyroidism. It may occur in those with established hypothyroidism when they develop an acute illness. Myxedema coma can be the first presentation of hypothyroidism. People with myxedema coma typically have a low body temperature without shivering, confusion, a slow heart rate and reduced breathing effort. There may be physical signs suggestive of hypothyroidism, such as skin changes or enlargement of the tongue.
Pregnancy
Even mild or subclinical hypothyroidism leads to possible infertility and an increased risk of miscarriage. Hypothyroidism in early pregnancy, even with limited or no symptoms, may increase the risk of pre-eclampsia, offspring with lower intelligence, and the risk of infant death around the time of birth.Women are affected by hypothyroidism in 0.3–0.5% of pregnancies. Subclinical hypothyroidism during pregnancy is associated with gestational diabetes, low birth-weight, placental abruption, and the birth of the baby before 37 weeks of pregnancy.
Pathophysiology
The hypothalamic-pituitary-thyroid axis governs thyroid hormone secretion (see the image below).
Although hypothalamic or pituitary disorders can affect thyroid function, localized disease of the thyroid gland that results in decreased thyroid hormone production is the most common cause of hypothyroidism. Under normal circumstances, the thyroid releases 100-125 nmol of T4 daily and small amounts of T3. The ratio of T4:T3 production varies between about 14:1 and 4:1, depending on iodine sufficiency and TSH stimulation. The half-life of T4 is approximately 7-10 days, whereas the half-life of T3 is about 24 hours. T4, a prohormone, is converted via the action of deiodinases to T3, the active form of thyroid hormone.
Early in the disease process, compensatory mechanisms maintain T3 levels. Decreased production of T4 causes an increase in the secretion of TSH by the pituitary gland. TSH stimulates hypertrophy and hyperplasia of the thyroid gland and 5’-deiodinase activity, thereby increasing T3 production.
Deficiency of thyroid hormone has a wide range of effects. Systemic effects are the result of either derangements in metabolic processes or direct effects by myxedematous infiltration (ie, accumulation of glycosaminoglycans in the tissues).
The hypothyroid changes in the heart result in decreased contractility, cardiac enlargement, pericardial effusion, decreased pulse, and decreased cardiac output.
In the gastrointestinal (GI) tract, achlorhydria and prolonged intestinal transit time with gastric stasis can occur in hypothyroidism. Non-alcoholic fatty liver disease (NAFLD) may also be significantly associated with hypothyroidism, as shown in a meta-analysis of 44,140 individuals with diagnosed hypothyroidism.
Delayed puberty, anovulation, menstrual irregularities, and infertility are common. TSH screening should be a routine part of any investigation into menstrual irregularities or infertility.
Patient Education
Emphasize proper compliance at each visit. Clearly discuss the lifelong nature of hypothyroidism, the need for lifelong levothyroxine therapy, the proper way to take medicine, and the need for TSH testing at least annually.
Patients should take thyroid hormone as a single daily dose. Thyroid hormone is better absorbed in the small bowel; therefore, absorption can be affected by malabsorptive states, small bowel disease (eg, celiac sprue), and the patient’s age. Many drugs (eg, iron, calcium carbonate, calcium acetate aluminum hydroxide, sucralfate, raloxifene, and proton pump inhibitors) can interfere with absorption and therefore should not be taken within 2-4 hours of LT4 administration. Continuous tube feedings interfere with thyroid hormone absorption; the tube feedings should be interrupted for at least 30-60 minutes before and after hormone administration.
For patients with malabsorption issues, such as those with celiac disease, Helicobacter pylori infection, lactose intolerance, inflammatory bowel disease, atrophic gastritis, or status post bariatric surgery, liquid LT4 formulations may be more efficient than tablet form for replacement and suppressive therapy. For those without malabsorption, either form is sufficient.
The effects of using softgel LT4 may also prove beneficial in malabsorptive states, and its effects have been found to be consistent with the liquid formulation. For both liquid and softgel LT4 formulations, cost is often a limiting factor for use.











